
Achilles Tendon Rupture (ATR) Rehab from Surgery to Return to Sport Continuum
June 2025
Achilles tendon ruptures (ATR) are among the most dramatic injuries in sport, often occurring during explosive movements like sprinting or jumping. While surgical repair is often necessary, the real challenge lies in the recovery. With our expertise in both physical therapy and strength and conditioning, PFP emphasizes a rehab process that not only protects the repair but prepares the athlete for high-level performance from the get go. In this blog, we outline our four-phase model to bridge the gap between rehabilitation and return to sport.
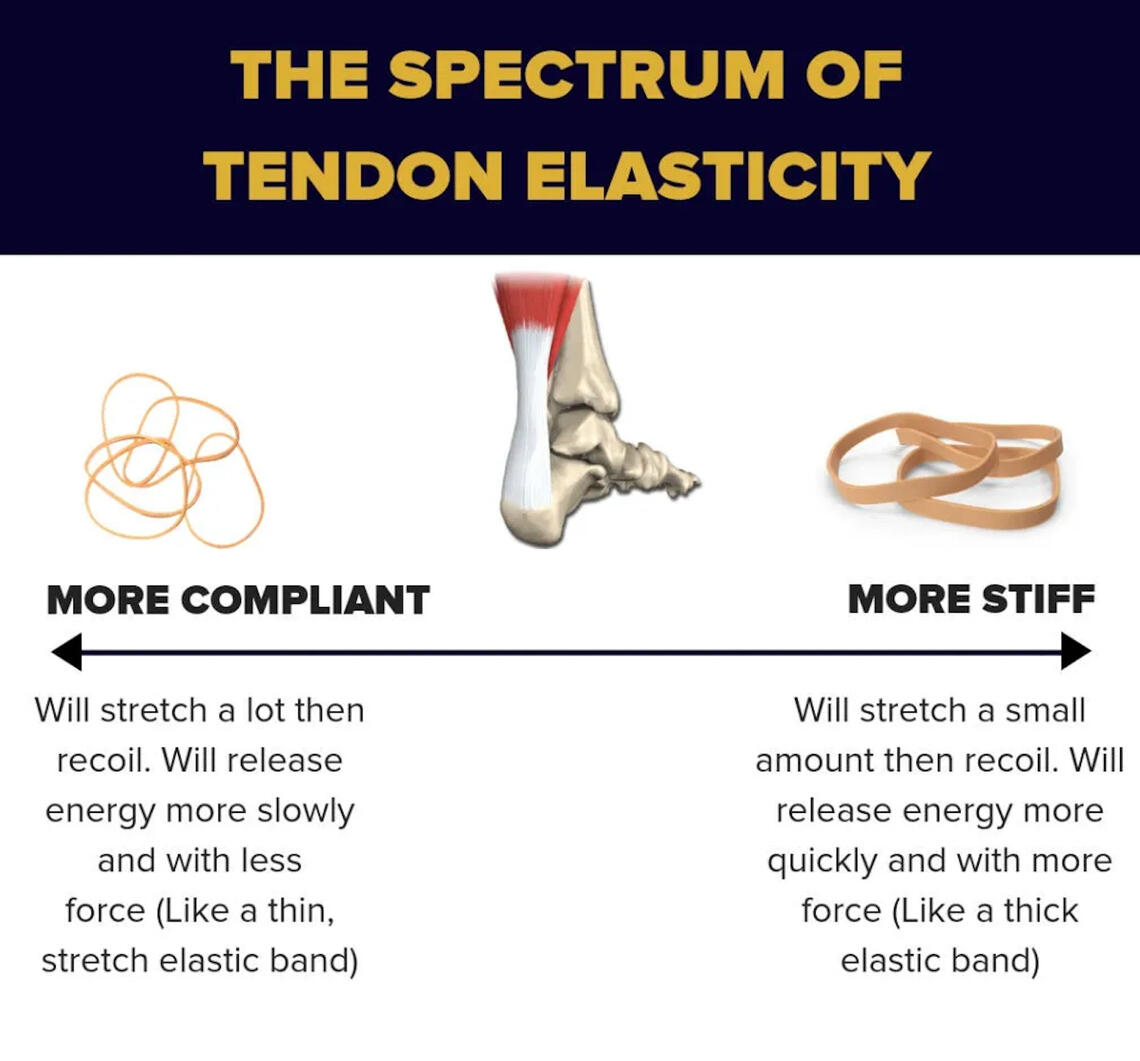
WHY ARE TENDONS UNIQUE?Tendons connect muscles to bones and are primarily composed of type I collagen fibers. They have a remarkable capacity to absorb and transmit force. Tendons operate on a spectrum of stiffness and elasticity. The stiffer the tendon, the better it can produce strength and power. The more elastic the tendon, the more it can act like a dynamic spring — stretching and recoiling — which is especially beneficial for change of direction (COD) movements such as jumping and cutting.

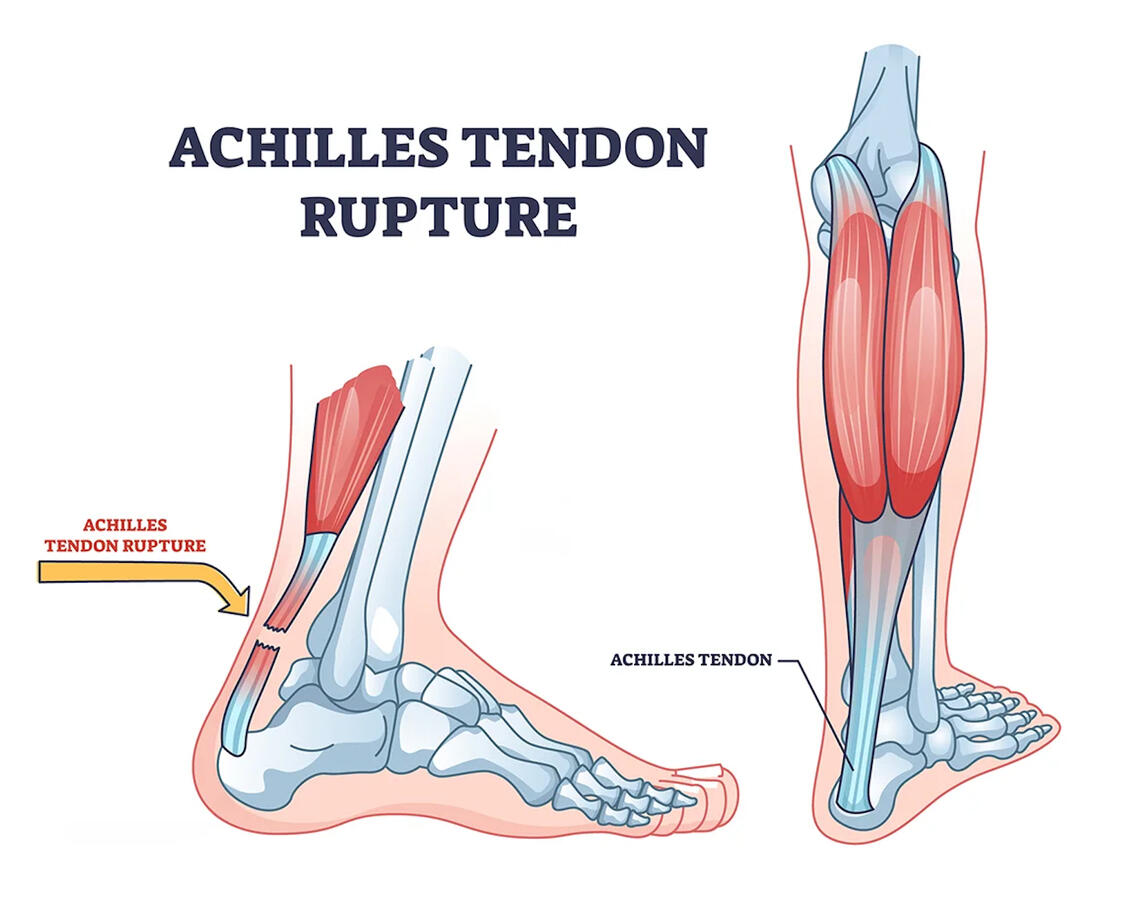
ACHILLES TENDON RUPTUREThe Achilles tendon must be both stiff and spring-like to generate force and facilitate efficient propulsion. It commonly tears higher up from its insertion on the calcaneus (heel bone). The typical mechanism of injury (MOI) involves the lower extremity moving into eccentric dorsiflexion, where the calf is lengthening under tension, followed by a rapid transition into concentric plantarflexion as the athlete attempts to push off. During this quick sequence, the combination of bodyweight and force production can exceed the tendon’s threshold for load, leading to a rupture. The characteristic 'pop' often reported with an ATR is the result of that excessive energy being released—according to the law of conservation of energy, the force that would have gone into the tendon is converted into sound.Following rupture, the tendon structure is compromised, shifting from strong type I collagen to weaker type III collagen. Without proper loading, the healing tendon may remain fragile. Smart, progressive loading is essential to restore tissue resilience and function.
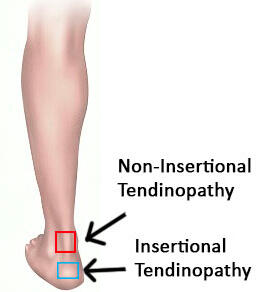
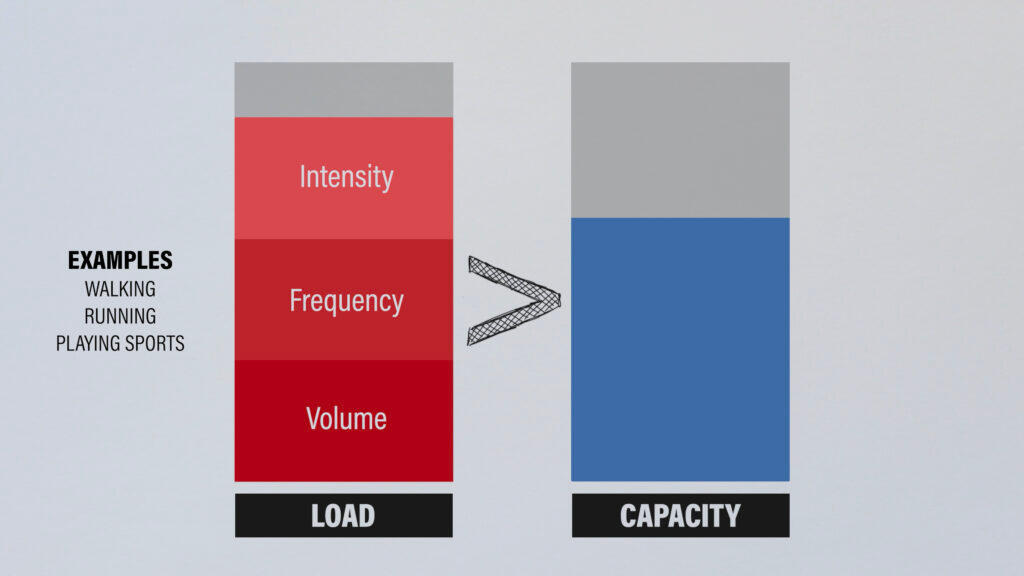
CAN ACHILLES TENDONITIS TURN INTO AN ACHILLES RUPTURE?Achilles tendinopathy is often the result of repetitive overloading, frequently caused by training errors like a sudden spike in intensity or volume. In fact, between 60% to 80% of individuals with Achilles tendinopathy develop it following rapid changes in training loads or inadequate recovery strategies (Silbernagel et al., 2015).There are two main types of Achilles tendinopathy:
1) Non-insertional (midportion): Typically occurs 2 to 6 cm above the calcaneus and presents with pain during activity and morning stiffness.2) Insertional: Felt directly around the calcaneus, usually where the tendon attaches to the bone.One of the biggest concerns in athletes with chronic tendinopathy is the risk of reinjury. In soccer players, for example, reinjury rates can range from 27% to 44%, especially when the return-to-sport process is rushed or lacks proper progressive overload (Silbernagel et al., 2015).But can Achilles tendinopathy actually progress to a full rupture? Yasui et al., 2017 analyzed 7,232 patients and found that roughly 4% of individuals with a diagnosis of Achilles tendinopathy went on to experience a complete rupture.
Here’s the key takeaway: pain with tendon loading is not something to ignore, especially in the context of high-stress movements like sprinting, jumping, or sudden deceleration.
PT PHASES OF REHAB

Phase I: Protection & Foundation (0-2 Weeks Post-Op)Goal: Protect the repair, manage swelling, restore gentle motion
- Weightbearing as prescribed (WBAT/NWB), walking boot with heel lifts
- Initiate gentle PROM, joint mobilizations, and scar mobilization techniques
- Activate foot intrinsics; perform ankle circles, hip, and core strengthening
- Cross-Education: Begin strength training on the non-injured side to enhance neural drive to the healing limb
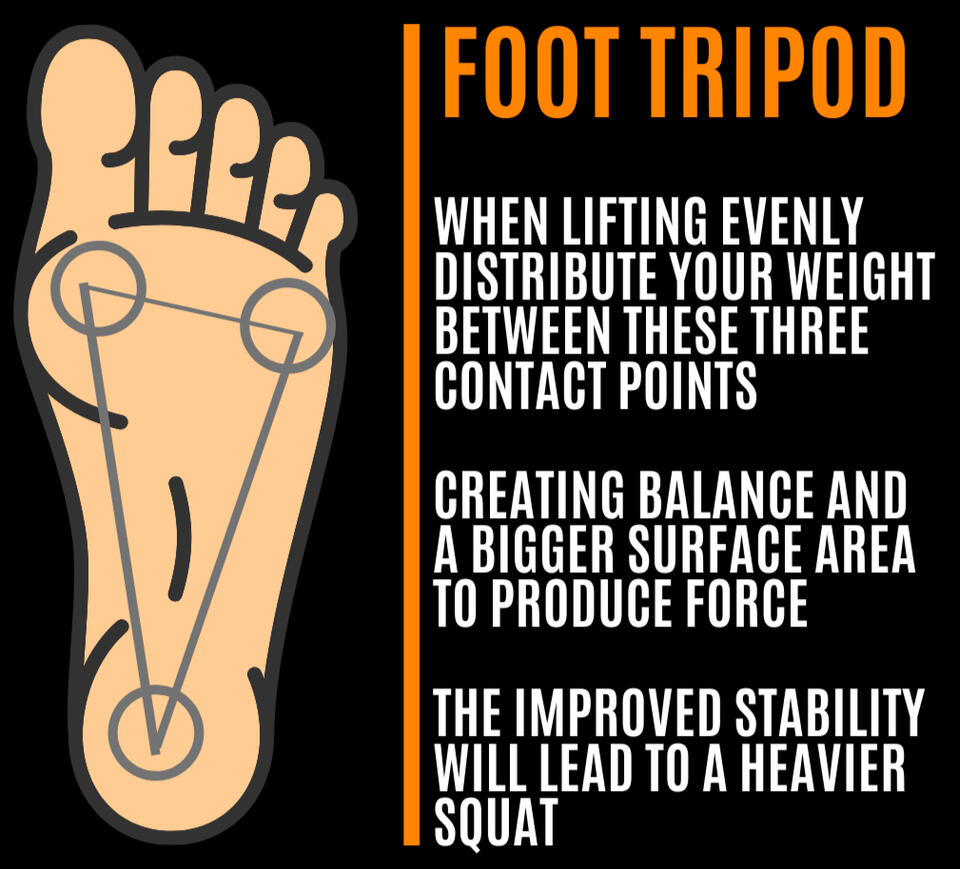
- Re-analyze the mechanics that contributed to the ATR, restore relative motions up the chain, and begin reinforcing more foundational movement patterns (i.e. tripod foot, hip shifts and anchoring, shin rotation, etc.)Early tendon loading should be subtle and strategic. Overload too soon = risk. Too cautious = poor remodeling.
Phase II: Early Loading (2-6 Weeks)Goal: Stimulate collagen formation, introduce isometrics
- Controlled active range of motion (AROM) in plantarflexion, inversion, and eversion
- Begin ankle isometrics, including isometric heel raises
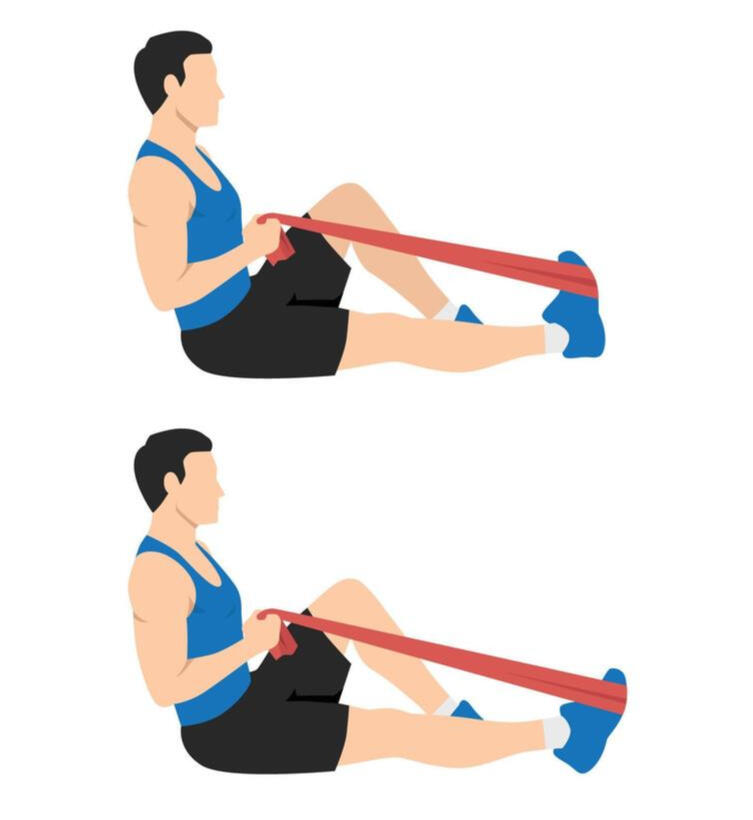
- Perform 4-way ankle resistance exercises using manual resistance and theraband as tolerated
- Progressively rebuild tendon strength through proper loading techniques
- Emphasize safe proprioceptive training with balance pads and controlled weight shifting with reintroduction of push off on affected sideDr. Keith Baar's research: Limited range of motion exercises, even with light loads, can effectively increase collagen synthesis during early connective tissue development. Early tendon cells respond best to short bursts of load—about 6–10 minutes total of isometric work—regardless of load amplitude (Baar et al., 2017)


Phase III: Strength & Capacity (6-12 Weeks)Goal: Build muscle, restore full ROM, improve force absorption
- Resistance training focused on slow eccentrics, eccentric loading, and overcoming isometrics (pushing against an immovable object)
- Calf raise progression (bent and straight knee), dynamic footwork drills
- Direct Hip and knee strength work, including split squat and variations, Romanian Deadlifts (RDL’s) and variations, step-downs and variations, etc.Return to Jogging Criteria:
- 25 single leg (SL) heel raises w/ <20% height difference
- 95% dorsiflexion and plantarflexion symmetry
- Gait and mechanics normalizedContinue restoring tibial, femoral, and pelvic relative motion to avoid compensation up the chain and to ensure smooth transition into phase 4
Keith Barr Tendon Model LoadingDr. Baar and Dr. Cook, two pioneers in tendon rehab, recommend progressing to heavy (> 80% of 1RM) isometric holds lasting about 30 seconds in a neutral joint position, accumulating a total of 5 minutes during this rehab phase. Why 30 seconds? Healthy collagen in the tendon can “stress shield” weaker regions, reducing load and collagen synthesis in the injured area. The 30-second duration allows stress relaxation to occur—where tendon force gradually decreases under a constant length and static load. This relaxation lets the stronger tendon fibers unload, directing mechanical signals specifically to the injured region. As a result, collagen re-synthesis is stimulated, promoting targeted tendon healing and rebuilding.



Phase IV: Return to Practice → Return to Sport → Return to Performance (12+ Weeks)KEY: Reconceptualize phase 4 as a return to sport continuum for athletes → return to practice in a controlled environment, return to sport on a pitch count, return to sport with no limitations, then working to return to prior level of performance, and finally surpassing previous level of performanceGoal: Restore full ROM, normalize gait and running mechanics, and progress to advanced tasks such as cutting, jumping, and both absorbing and producing high levels of force.
Initiate plyometric training, prioritizing force absorption before progressing to force production
- Plyometric loading targets the tendon’s elastic capacity; training both slow plyometrics for brute force production and fast plyometrics to tap into the stretch-shortening cycles (SSC) are essential to meet the stiffness and elasticity demands of the Achilles tendon
- Continue progressing strength training from Phase III
- Develop sport-specific capacity for speed, deceleration, and agility, ensuring proper mechanics throughoutReturn to Sport Testing:
- Less than 10% plantarflexion strength asymmetry at 0º dorsiflexion
- Adequate neuromuscular control (e.g., at least 90% symmetry on the Y-Balance Test)
- Physician clearance and confidence in movement
The PFP DifferenceThis only scratches the surface of the complexities involved in Achilles tendon rupture (ATR) rehabilitation. At PFP, our approach is always tailored to each individual’s unique deficits, limitations, presentation, goals, and sport-specific demands.We don’t just help athletes return to activity—we prepare them to perform. Our model combines clinical reasoning with advanced strength and conditioning principles to ensure a safe, confident, and complete return to peak performance.
